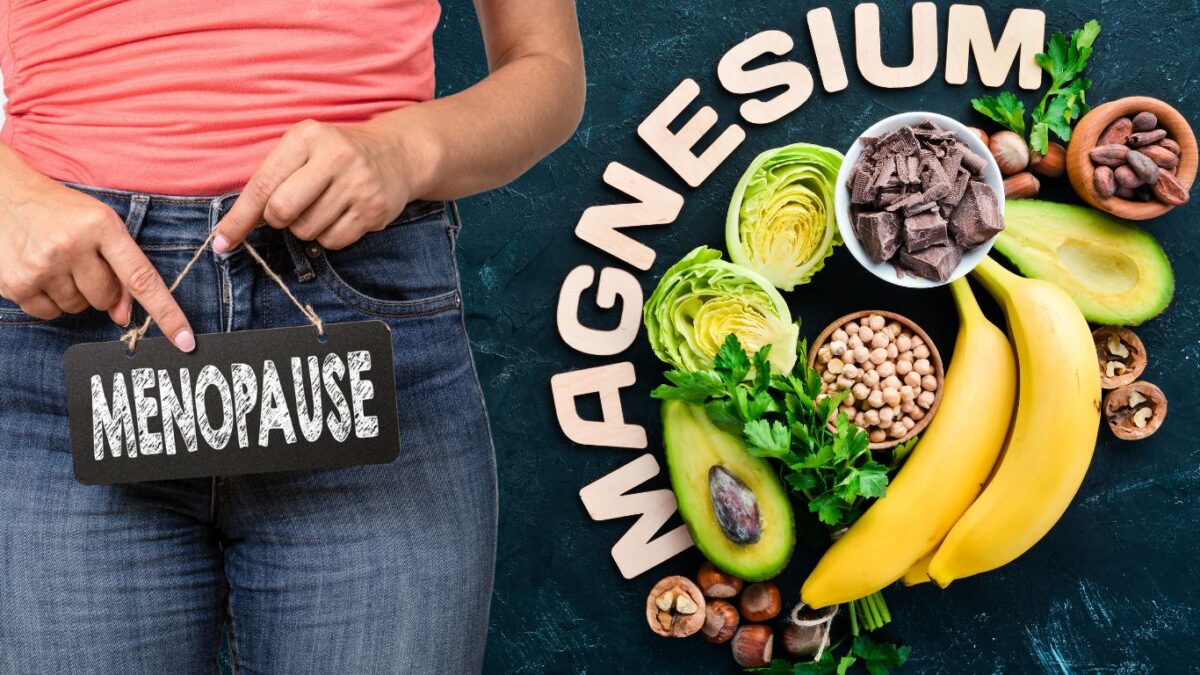
Missing Magnesium in Menopause? The Essential Mineral You Need Now
Among all the nutrients that play a crucial role during menopause transition, magnesium stands out for its extensive health benefits. It is a vital mineral that is involved in numerous biochemical processes in the body, contributing to bone health, mood stability, and cardiovascular wellness, among other aspects. Understanding the importance of magnesium in menopause is essential for women to deal with this phase with enhanced comfort and health. This blog explores the multifaceted role of magnesium in menopause, shedding light on its various benefits and how it aids in alleviating and managing menopausal symptoms and related health concerns.
Imagine it as a quiet but sturdy pillar, holding the fort in maintaining bone density and strength, crucial for warding off osteoporosis. This condition tends to sneak up on postmenopausal women, thanks to a significant dip in estrogen levels. But with magnesium on guard, there’s an extra layer of defense in place.
But that’s not all! Beyond bones, magnesium is a friend to your mood too. It plays a significant role in ensuring neurotransmitters function as they should, potentially keeping those unwelcome feelings of depression, anxiety, and irritability at arm’s length. It’s like having a friend by your side, helping you keep your cool amidst the menopausal whirlwind.
And when it comes to sleep, magnesium is the lullaby for your restless nights. It contributes to relaxation and partners with the sleep hormone melatonin to enhance sleep quality. If menopause has been playing havoc with your sleep, think of magnesium as the gentle hand rocking you back to peaceful slumber.
Let’s not forget the heart. Magnesium stands as a guardian for cardiovascular health, helping regulate blood pressure and heart rhythm, and in turn, working to reduce the risk of heart diseases that spike after menopause. It’s like having a vigilant watchman ensuring your heart beats with unwavering rhythm.
Experiencing hot flashes and night sweats? Magnesium steps up once again, possibly helping manage these vasomotor symptoms, making the menopausal transition a tad more comfortable. It’s akin to a gentle breeze in the heat, offering respite and comfort.
And there’s more. Magnesium is also in the mix, ensuring hormonal balance and aiding in muscle function, reducing cramps and managing muscle discomfort that can rear its head during menopause. It’s like a soothing balm, easing the aches and keeping the balance in check.
Embracing magnesium-rich foods or supplements could be a game-changer in managing various symptoms and health concerns associated with menopause. Here are some foods that are high in magnesium and can be beneficial during menopause:
1. Leafy Green Vegetables:
- Examples: Spinach, Swiss chard, and kale.
- Benefits: Besides magnesium, they are also packed with other essential nutrients and antioxidants.
2. Nuts and Seeds:
- Examples: Almonds, pumpkin seeds, sunflower seeds, and chia seeds.
- Benefits: They are also a good source of healthy fats, protein, and fiber.
3. Whole Grains:
- Examples: Quinoa, brown rice, and whole wheat.
- Benefits: Whole grains also provide other essential nutrients and are a good source of fiber.
4. Fish:
- Examples: Mackerel, salmon, and halibut.
- Benefits: Fish is also rich in omega-3 fatty acids which are good for heart health.
5. Legumes:
- Examples: Black beans, chickpeas, and lentils.
- Benefits: Legumes are also high in protein and fiber.
6. Dark Chocolate:
- Benefits: Besides being a delicious treat, dark chocolate is also rich in antioxidants.
7. Avocado:
- Benefits: Avocados are also a good source of potassium, vitamins, and healthy fats.
8. Bananas:
- Benefits: Bananas are a convenient snack and also provide other essential vitamins and minerals.
9. Yogurt:
- Benefits: Yogurt is also a good source of calcium and probiotics.
10. Dried Fruits:
- Examples: Figs and apricots.
- Benefits: Dried fruits are also high in fiber and antioxidants.