Hair Loss in Perimenopause & Menopause: Causes and Effective Remedies
Hair loss during perimenopause and menopause is a common yet distressing experience for many women. As hormone levels shift, you may notice thinning hair, excessive shedding, or even bald spots. While losing around 100 hairs per day is normal, menopause-related hair loss often feels more dramatic due to slower regrowth.
If you’re in your 40s or 50s and wondering why your hair is thinning, don’t worry—you’re not alone! The good news is that several remedies and treatments can help manage hair loss and promote healthier, fuller hair. In this blog, we’ll explore the causes of menopausal hair loss and the best natural remedies, medical treatments, and lifestyle changes to keep your hair looking its best.
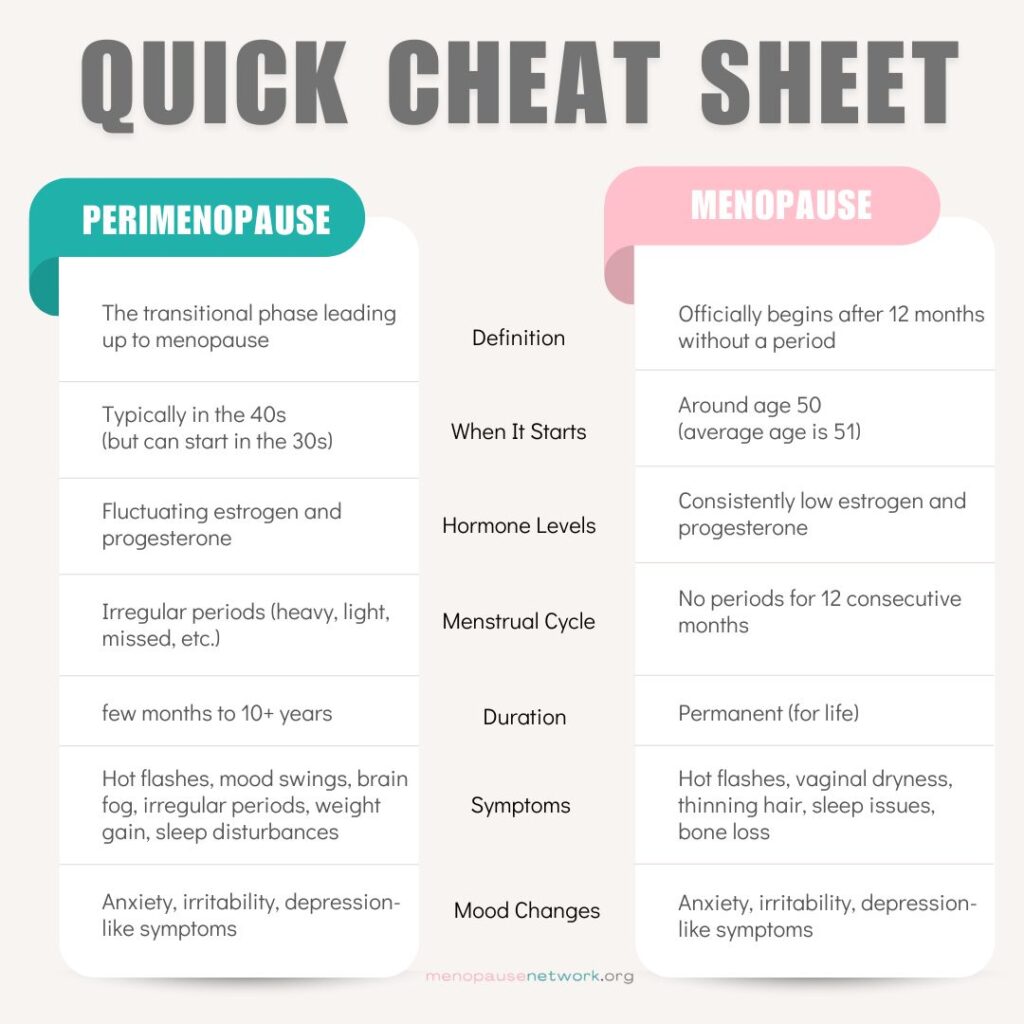
Causes of Hair Loss During Perimenopause & Menopause
1. Hormonal Imbalance (Estrogen Decline & Increased Androgens)
- Estrogen helps keep hair in the growth phase, but during perimenopause and menopause, estrogen levels drop.
- At the same time, androgens (male hormones) may increase, causing hair thinning, especially at the crown and temples.
2. Stress & Cortisol Spikes
- Menopause is often a stressful transition, and chronic stress increases cortisol levels, which can disrupt hair growth cycles.
- Telogen Effluvium: A condition where stress pushes hair into the shedding phase too soon, causing noticeable thinning.
3. Nutrient Deficiencies
- Iron, vitamin D, B vitamins, zinc, and biotin are all crucial for hair health.
- Many women experience iron deficiency due to heavy periods before menopause or insufficient dietary intake.
- A low-protein diet can also lead to weaker hair strands and increased breakage.
4. Thyroid Imbalances
- Menopausal hormonal shifts can sometimes trigger hypothyroidism (underactive thyroid), which causes hair thinning, dryness, and breakage.
- If you notice fatigue, weight gain, or brittle nails along with hair loss, a thyroid test may be needed.
5. Medications & Medical Treatments
- Certain medications prescribed during menopause, such as hormone replacement therapy (HRT), blood pressure meds, or antidepressants, can contribute to temporary hair shedding.
- Chemotherapy and radiation treatments can also accelerate hair loss.
6. Scalp Health & Hair Styling Habits
- Dandruff, inflammation, or scalp infections can weaken hair follicles.
- Frequent blow-drying, straightening, or using chemical treatments can worsen breakage and thinning.
- Tight hairstyles, such as ponytails and buns, can cause traction alopecia (hair loss due to tension on the scalp).
Remedies for Menopausal Hair Loss
1. Scalp Massage with Essential Oils
- Massaging your scalp for 5-10 minutes daily can improve blood circulation and support hair regrowth.
- Use rosemary oil, peppermint oil, or castor oil—these are known to strengthen hair follicles and promote thickness.
2. Biotin & Collagen Supplements
- Biotin (Vitamin B7) supports keratin production, the protein essential for strong hair.
- Collagen supplements help maintain hair elasticity and reduce breakage.
3. Hormone Therapy (HRT or Natural Supplements)
- Hormone Replacement Therapy (HRT) can help some women regain hair density by restoring estrogen levels.
- If HRT isn’t an option, phytoestrogens (found in soy, flaxseeds, and red clover) may help balance hormones naturally.
4. Protein-Rich Diet for Stronger Hair
- Eating lean proteins like fish, eggs, tofu, lentils, and nuts helps repair damaged hair strands.
- Omega-3 fatty acids (found in salmon, chia seeds, and walnuts) keep the scalp hydrated and reduce inflammation.
5. Minoxidil (FDA-Approved Treatment for Female Hair Loss)
- Minoxidil (Rogaine) is a topical treatment proven to regrow thinning hair.
- It works by extending the hair growth phase and increasing follicle size.
- Results take about 3-6 months, and continuous use is needed for long-term benefits.
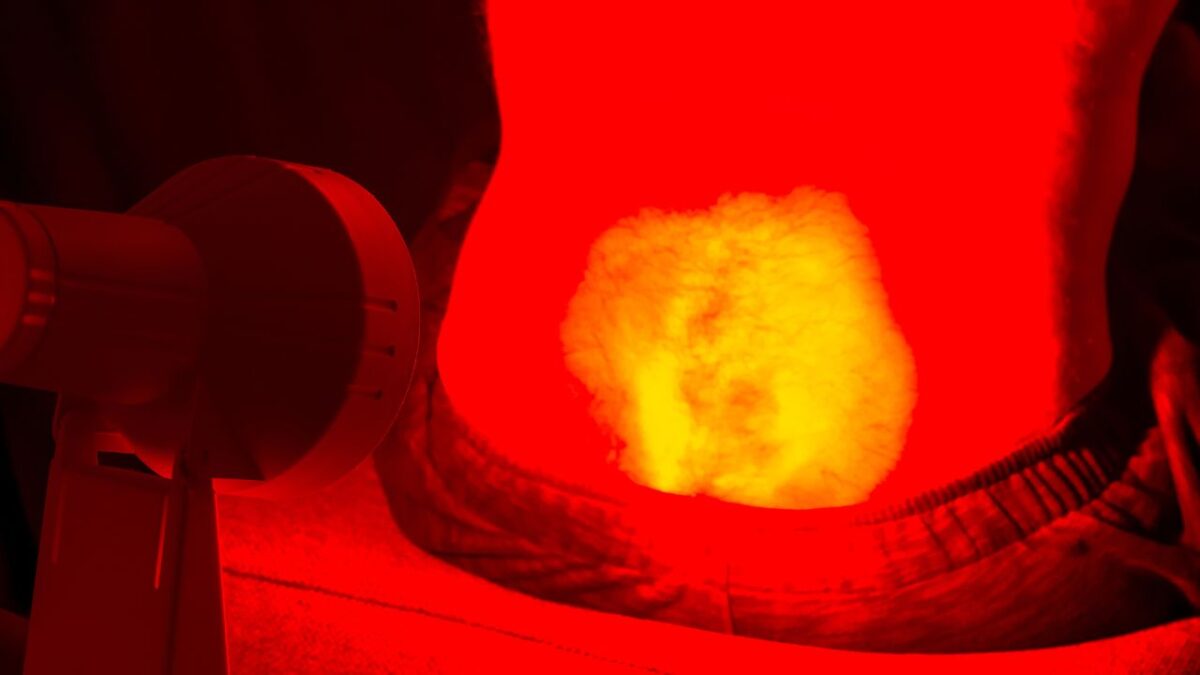
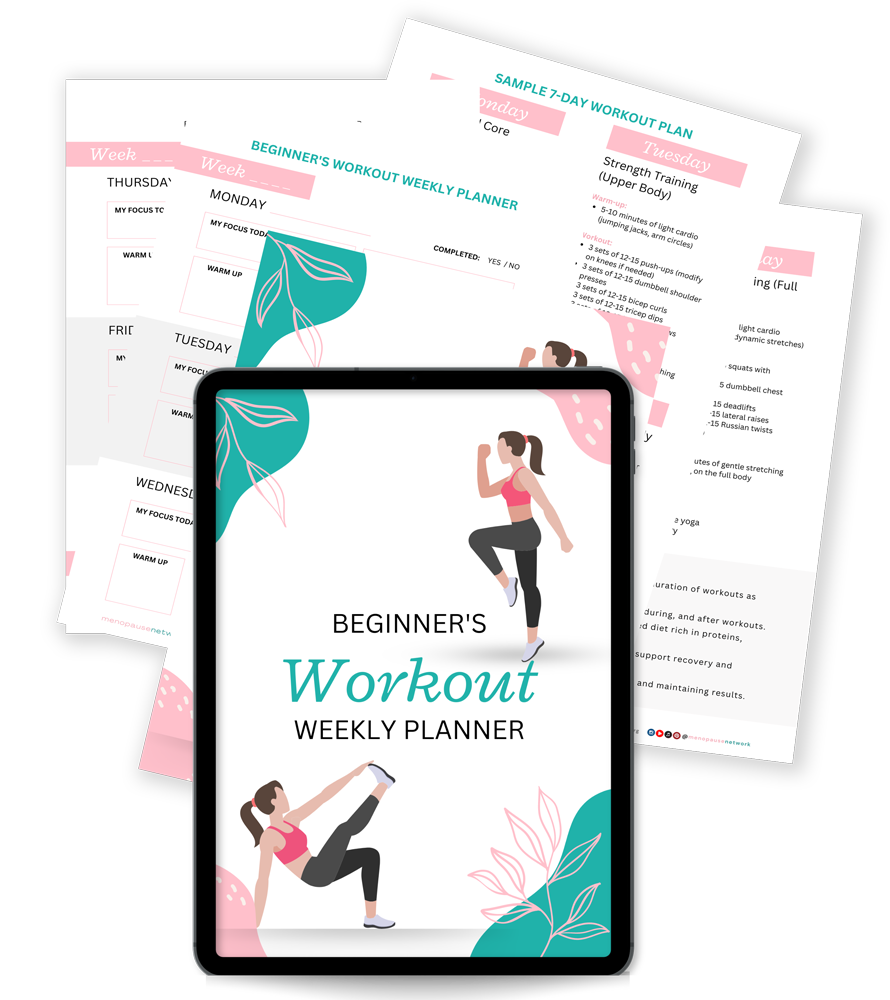
6. Stress Reduction (Yoga, Meditation & Self-Care)
- Managing stress is key to reducing cortisol levels and preventing further hair loss.
- Engage in gentle exercise, deep breathing, and mindfulness practices to support overall well-being.
7. Onion Juice (Surprising Natural Remedy!)
- Onion juice contains sulfur, which improves collagen production and strengthens hair follicles.
- A 2002 study found that applying onion juice twice daily helped hair regrowth in 6 weeks.
- Downside? The strong smell! Be sure to rinse thoroughly after applying.
8. Herbal Remedies (Ginseng & Saw Palmetto)
- Ginseng stimulates hair follicle activity and may help promote regrowth.
- Saw Palmetto blocks DHT (a hormone linked to hair loss), which may slow menopause-related thinning.
9. Gentle Hair Care Routine
- Use sulfate-free shampoos to avoid stripping natural scalp oils.
- Try volumizing shampoos with keratin and biotin to strengthen hair strands.
- Avoid heat styling, harsh chemical treatments, and tight hairstyles.
10. Hair Transplant (For Severe Hair Loss)
- If hair thinning is advanced and persistent, a hair transplant may be an option.
- This surgical procedure relocates hair follicles from other parts of the scalp to thinning areas.
Conclusion
Hair loss during perimenopause and menopause is a common but manageable concern. The key to preserving healthy hair is understanding the underlying hormonal, nutritional, and lifestyle factors contributing to hair thinning.
💡 Simple changes like eating a protein-rich diet, reducing stress, massaging your scalp, and using targeted treatments like Minoxidil or biotin can make a noticeable difference.
If your hair loss is severe or sudden, consulting a doctor or dermatologist is essential to rule out thyroid imbalances, iron deficiencies, or other medical conditions.