Joint Health for Women: Simple Tips to Ease Aches and Pains
Joint pain can be more than a minor annoyance—it’s a roadblock to enjoying your everyday life. From the stiffness that greets you in the morning to the aches after sitting too long, joint discomfort can weigh you down. But here’s the good news: there are simple and natural ways to feel more flexible, strong, and ready to take on your day. Let’s dive into what you can do to keep your joints happy and healthy.
Common Causes of Joint Pain in Women
If you’re wondering why your joints hurt, there’s no one-size-fits-all answer. For women, joint pain often arises from a mix of factors, including:
- Arthritis: Conditions like osteoarthritis and rheumatoid arthritis become more common with age.
- Hormonal Shifts: Estrogen, which supports joint health, declines during menopause, potentially leading to pain and inflammation.
- Lifestyle Choices: Excess weight, lack of exercise, or repetitive movements can put stress on your joints.
- Autoimmune Conditions: Disorders like lupus or fibromyalgia can also play a role.
Understanding the cause is the first step to finding relief. Be sure to check in with a healthcare professional for an accurate diagnosis.
Keep Moving: Why Staying Active Helps Your Joints
When your joints hurt, it’s tempting to skip exercise—but staying active can actually help ease the pain. Movement keeps your joints flexible and strengthens the muscles that support them.
Gentle Exercises for Joint Health:
- Low-Impact Activities: Swimming, walking, or yoga are easy on your joints while improving mobility.
- Strength Training: Building muscle reduces pressure on your joints. Start small and gradually increase the weight.
- Stretching: Pilates or simple stretches can help reduce stiffness and improve range of motion.
The key? Find an activity you enjoy and make it a daily habit. Even short sessions can make a big difference.
Natural Ways to Soothe Joint Pain
Looking for natural solutions? These tried-and-true tips can help:
Eat for Joint Health:
- Anti-Inflammatory Foods: Think omega-3-packed salmon, leafy greens, and antioxidant-rich berries.
- Cut the Junk: Limit processed foods, refined carbs, and sugar that can worsen inflammation.
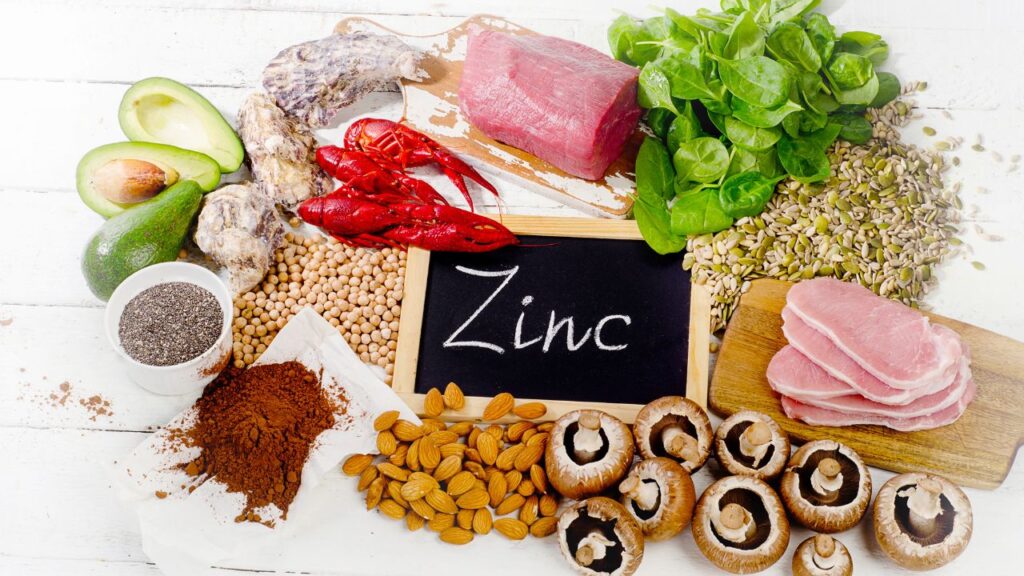
- Supplements: Glucosamine, chondroitin, and turmeric are popular choices for joint health.
Stay Hydrated:
Cartilage is about 80% water, so drinking plenty of water helps cushion your joints and reduce friction.
Try Home Remedies:
- Epsom Salt Baths: The magnesium in Epsom salts can relax muscles and reduce inflammation.
- Essential Oils: Peppermint or eucalyptus oils provide soothing relief when applied to sore areas.
- Herbal Teas: Ginger and turmeric teas are anti-inflammatory powerhouses.
Lifestyle Tweaks for Healthier Joints
A few small changes to your daily routine can work wonders for your joint health:
- Maintain a Healthy Weight: Shedding even a few pounds reduces stress on your joints, especially in your knees and hips.
- Prioritize Sleep: Your body repairs itself while you sleep. Invest in a supportive mattress and consider natural sleep aids like magnesium if pain keeps you up.
- Listen to Your Body: Pain is your body’s way of saying something isn’t right. Don’t ignore it—rest or seek medical advice when needed.
Takeaway
Joint pain doesn’t have to control your life. With a mix of movement, smart lifestyle choices, and natural remedies, you can take charge of your joint health and get back to doing what you love. Remember, consistency is key—a little effort each day goes a long way toward healthier, pain-free joints.