The $275 Million Step Towards Revolutionizing Midlife Women’s Health
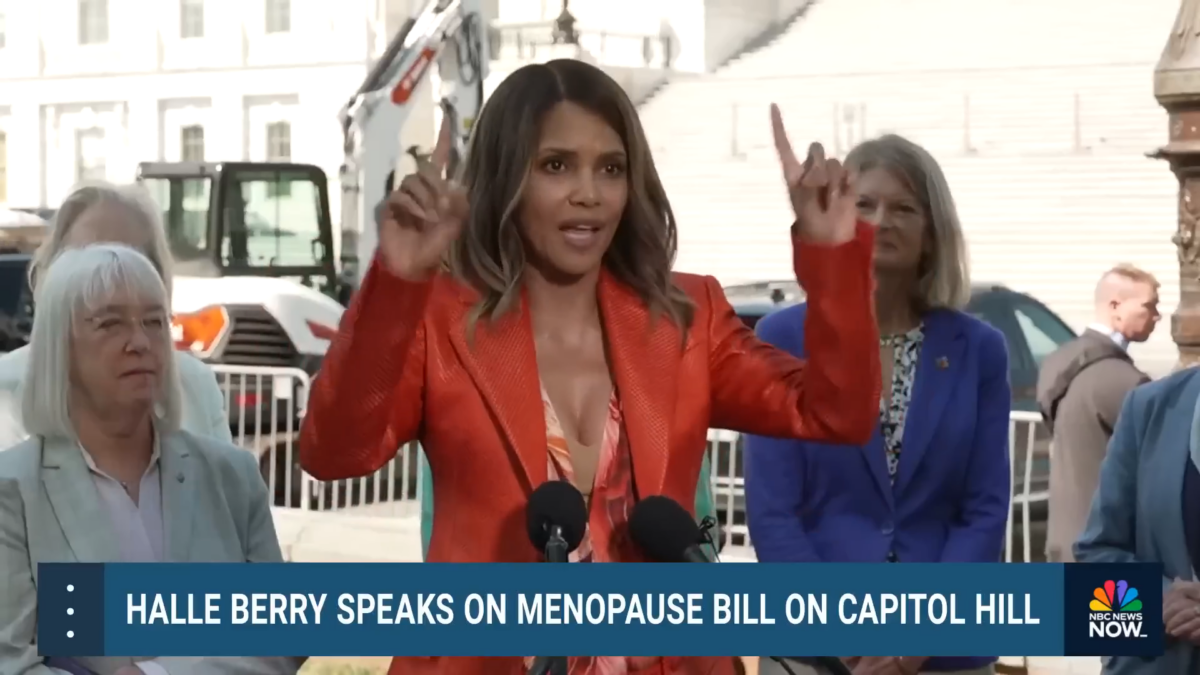
Just recently, Hollywood Actress Halle Berry has collaborated with a bipartisan group of U.S. senators to introduce this bill which aimed at enhancing menopause and midlife women’s health research, training, and public awareness. The legislation, titled the Advancing Menopause Care and Mid-Life Women’s Health Act, proposes a $275 million investment over five years. It includes funding for research, public health promotion, professional training, and establishing Centers of Excellence in Menopause and Mid-Life Women’s Health. Berry, highlighting her personal struggles with menopause misdiagnoses, emphasized the non-political nature of this issue and its significance as a human rights concern. The bill has gained broad support across the political spectrum, reflecting a growing acknowledgment of the need for focused attention on women’s health issues that have historically been marginalized.
Here’s a breakdown of its key aspects:
Focus Areas:
- Research: The Act calls for increased federal funding for research on menopause, including evaluating existing research and identifying gaps in knowledge regarding treatments and their effectiveness.
- Education and Awareness: It aims to raise awareness about menopause and mid-life health issues through educational initiatives for healthcare professionals and the public.
- Healthcare Workforce Training: The Act emphasizes the need for better training for healthcare providers on managing menopause and related symptoms.
- Public Health Promotion: It encourages preventative measures and public health initiatives to address potential health risks associated with menopause.
Overall Goal:
The Act strives to improve the overall experience of menopause for women by:
- Strengthening research: Leading to the development of more effective treatment options.
- Enhancing education and awareness: Empowering women to manage their symptoms and make informed decisions about their health.
- Equipping healthcare providers: Ensuring women have access to qualified professionals who can effectively address their menopause-related concerns.
- Promoting preventative measures: Helping women maintain good health during menopause and beyond.
Current Status (as of May 14, 2024):
The Advancing Menopause Care and Mid-Life Women’s Health Act was introduced in December 2023 and is currently under consideration by the U.S. Congress.
The Impact on Women
The Advancing Menopause Care and Mid-Life Women’s Health Act has several potential impacts on women, especially those experiencing menopause and related mid-life health concerns. Here’s how it could affect women:
- Improved Treatments and Symptom Management:
- By boosting research funding, the Act would facilitate a deeper understanding of menopause and its symptoms. This could lead to the development of more effective and personalized treatments, helping women manage symptoms such as hot flashes, sleep disturbances, and mood swings more effectively.
- Increased Awareness and Education:
- The focus on educational initiatives would help demystify menopause for both the public and healthcare providers. Increased awareness could reduce the stigma and misconceptions surrounding menopause, making it easier for women to seek help and discuss their health openly.
- Better Healthcare Experiences:
- Training healthcare providers specifically about menopause management means that women are more likely to receive informed, empathetic care tailored to their needs. This can improve the overall healthcare experience for women at mid-life, making it more likely that they receive timely and effective interventions.
- Enhanced Public Health Measures:
- Promoting public health initiatives related to lifestyle adjustments and preventative care can help women address and potentially reduce the risks associated with menopause-related health issues, such as cardiovascular disease and osteoporosis.
- Empowerment and Informed Decision-Making:
- With increased education and resources, women are better equipped to make informed decisions about their health. Understanding their own bodies and the changes occurring during menopause can empower women to advocate for themselves in healthcare settings and in their personal health choices.
- Long-Term Health Benefits:
- Preventative health measures and education can have long-term benefits by encouraging healthier lifestyles and proactive health management. This can lead to a reduction in chronic conditions often exacerbated by menopause, such as diabetes and hypertension.
Overall, if effectively implemented, the Advancing Menopause Care and Mid-Life Women’s Health Act could significantly enhance the quality of life for women experiencing menopause, leading to better health outcomes and a more supportive healthcare environment. This could also set a precedent for how menopause and women’s health issues are handled in other regions or countries.