Struggling with Hair Loss During Menopause? Here Are the Top 8 Natural Solutions!
For many, hair is not just about aesthetics; it is tied to self-identity and confidence. As women approach menopause, the experience of thinning hair or noticeable hair loss can lead to feelings of frustration and self-consciousness. Understanding the root causes of hair loss during this stage and exploring effective treatments becomes crucial.
While medical treatments and pharmaceutical options are available, many women prefer natural remedies that are gentler on the body and free from side effects. Natural remedies focus on holistic approaches that nurture the body and promote hair health from within. This comprehensive guide aims to provide practical, natural solutions to manage and potentially reverse hair loss during menopause.
From addressing chemical and physical damage to balancing hormones naturally, this guide delves into various treatment approaches. It emphasizes the importance of a healthy lifestyle, including proper nutrition, hydration, exercise, and stress management, which are all pivotal in maintaining hair health. By incorporating these natural remedies, women can take proactive steps to support their hair health during menopause, fostering both physical and emotional well-being.
In the following blog, we will explore in detail the causes of hair loss and provide practical, natural treatment approaches. Here are detailed approaches to help you combat hair loss naturally.
1. Stop the Damage
Avoid Chemical Treatments
- Herbal Hair Dyes: Switch to herbal hair dyes made from natural ingredients like henna, indigo, or chamomile. These dyes are gentler on the hair and do not damage the follicles.
- Natural Hair Styling: Opt for natural hair styling methods, such as using heat-free techniques like braiding or using rollers to achieve curls.
Loose Hairstyles
- Protective Hairstyles: Choose protective hairstyles that do not pull on the hair, such as loose braids, twists, or buns. These styles minimize tension and breakage.
- Silk or Satin Accessories: Use silk or satin hair accessories to reduce friction and prevent hair damage.
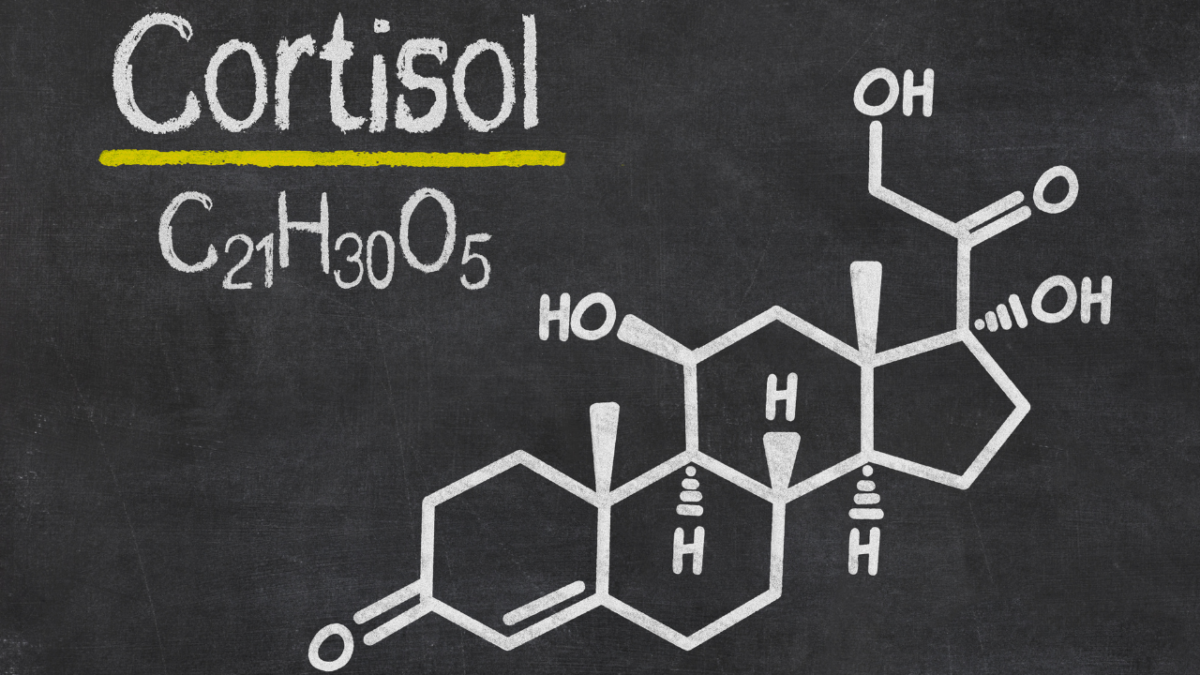
2. Balance Hormones
Natural Hormone Balancers
- Wild Yam Cream: This cream contains natural progesterone, which can help balance hormones. Apply it as directed to alleviate symptoms of hormonal imbalance.
- Herbal Supplements: Consider herbal supplements like black cohosh, red clover, and evening primrose oil, which are known to support hormonal balance during menopause.
3. Address Anemia
Increase Iron Intake
- Iron-Rich Foods: Incorporate iron-rich foods into your diet, such as spinach, lentils, chickpeas, pumpkin seeds, and quinoa. These foods help boost iron levels naturally.
- Vitamin C: Enhance iron absorption by consuming vitamin C-rich foods like oranges, strawberries, bell peppers, and broccoli alongside iron-rich meals.
Improve Hydrochloric Acid Levels
- Apple Cider Vinegar: Take a tablespoon of apple cider vinegar diluted in a glass of water before meals to improve stomach acid levels and aid iron absorption.
- Ginger Tea: Drink ginger tea regularly to stimulate digestive enzymes and improve overall digestion.
4. Scalp Treatments
Nourishing Oil Mix
- Coconut Oil: Known for its moisturizing properties, coconut oil can penetrate the hair shaft and nourish the scalp.
- Castor Oil: Castor oil is rich in ricinoleic acid, which can improve blood circulation to the scalp and promote hair growth.
- Rosemary Essential Oil: Rosemary oil is known to stimulate hair follicles and improve hair thickness. Mix a few drops into your oil blend.
Application:
- Mix equal parts coconut oil and castor oil.
- Add a few drops of rosemary essential oil.
- Warm the mixture slightly and massage it into your scalp.
- Leave it on for at least 30 minutes or overnight before washing it out with a gentle shampoo.
5. Exercise
Boost Circulation
- Yoga: Practicing yoga poses that increase blood flow to the scalp, such as downward-facing dog, can enhance hair health.
- HIIT: Incorporate high-intensity interval training (HIIT) into your routine. This form of exercise improves overall circulation and can promote hair growth.
6. Hydration
Drink Plenty of Water
- Hydration Goal: Aim to drink at least 8 glasses of water a day. Proper hydration keeps the scalp healthy and supports hair growth.
- Herbal Teas: Include herbal teas like nettle and horsetail, which are known for their hair-strengthening properties.
7. Nutrition
High-Fiber Diet
- Fiber-Rich Foods: Include foods like oats, barley, fruits, and vegetables in your diet to support overall health and hair growth.
- Protein and Healthy Fats: Ensure adequate intake of protein and healthy fats from sources like avocados, nuts, seeds, and olive oil. These nutrients are essential for hair health.
8. Proper Sleep
Establish a Sleep Routine
- Sleep Environment: Create a sleep-friendly environment by reducing noise, using comfortable bedding, and keeping the room dark and cool.
- Sleep Schedule: Maintain a regular sleep schedule by going to bed and waking up at the same time every day. Aim for at least 8 hours of sleep per night.
- Relaxation Techniques: Practice relaxation techniques such as meditation, deep breathing, or reading before bedtime to promote restful sleep.
Takeaway
Adopting natural remedies and holistic approaches can significantly help manage hair loss during menopause. By focusing on gentle, nourishing treatments and lifestyle changes, you can promote healthier hair growth and overall well-being. Remember to consult with a healthcare provider before starting any new treatments or making significant changes to your diet or lifestyle. Taking these proactive steps can lead to a noticeable improvement in hair health during menopause.