The Importance of Trace Minerals for Bone Health During Perimenopause
Navigating the perimenopausal journey is like embarking on a rollercoaster ride with unexpected twists and turns. As our bodies gracefully transition into a new phase, it’s crucial to pay attention to the unsung heroes that contribute to our overall well-being—trace minerals. In this blog post, we’ll be unraveling the mystery behind the vital role of trace minerals for bone health during perimenopause.
As women approach the perimenopausal stage, bone health becomes a key focal point. The body undergoes hormonal shifts that can affect bone density and increase the risk of osteoporosis. While we often hear about the importance of calcium and vitamin D, there are also trace minerals that quietly play a pivotal role in fortifying our skeletal foundation.
In this journey through the world of perimenopause and bone health, we’ll delve into the active mechanisms by which trace minerals operate. From facilitating collagen synthesis to boosting antioxidant defenses, these micronutrients are the unsung champions that deserve a spotlight.
So, fasten your seatbelts as we embark on a captivating exploration into the vital role of trace minerals for bone health during perimenopause. Let’s uncover the secrets that lie beneath the surface and empower ourselves with the knowledge to embrace this transformative phase with strength and vitality.
Why Tiny Minerals Matter Big Time
Alright, let’s set the scene. You’ve probably heard all about calcium and vitamin D for strong bones. But there’s more to the story – enter trace minerals! These little minerals might be in the background, but they’re doing some major work to keep your bones healthy and strong. We’re talking about magnesium, zinc, and boron – also known trace minerals for bone health.
Magnesium: Your Bone’s Best Friend

Magnesium is a vital trace mineral not just for maintaining healthy bones, but also for supporting overall physical health. Its roles in bone structure, vitamin D metabolism, and muscle and nerve function highlight its importance in a balanced diet. Regularly including magnesium-rich foods in your meals can help maintain optimal bone health and overall wellbeing.
What Magnesium Does for Your Bones
- Bone Structure and Strength: Magnesium is a crucial component of the bone matrix—the structure that gives bones their strength and stability. It works hand in hand with calcium and phosphorus, two other key minerals for bone health.
- Bone Cell Regulation: It plays a vital role in the activities of osteoblasts (cells that build bone) and osteoclasts (cells that break down bone). By regulating these cells, magnesium ensures a healthy balance between bone formation and bone breakdown.
- Enhancing Vitamin D Function: Magnesium is essential for converting vitamin D into its active form. Since vitamin D is crucial for calcium absorption, magnesium indirectly helps ensure that your bones get enough calcium.
Health Benefits Beyond Bones
- Muscle Function: Magnesium is also vital for muscle health, helping muscles contract and relax. This is important not just for movement, but also for supporting the muscles around your bones.
- Nerve Function: It plays a role in nerve function, helping transmit nerve signals throughout the body. This is crucial for coordinating muscle movements and maintaining overall bodily coordination.
- Heart Health: Magnesium contributes to heart health by regulating heartbeat and supporting the muscles in the heart.
Sources of Magnesium
- Dietary Sources: The best way to get magnesium is through your diet. Foods rich in magnesium include leafy green vegetables (like spinach and kale), nuts (especially almonds, cashews, and peanuts), seeds (like pumpkin seeds and chia seeds), whole grains (such as brown rice and whole wheat), and legumes (like black beans and lentils).
- Supplements: While diet is the best source, some people might need supplements, especially if they have a condition that affects magnesium absorption. However, it’s important to consult with a healthcare provider before starting any supplement regimen.
Recommended Intake
- Varies by Age and Gender: The recommended daily intake of magnesium varies depending on age, gender, and life stage. For example, adults generally need between 310 and 420 mg per day, but this can vary, especially for pregnant or breastfeeding women.
Signs of Magnesium Deficiency
- Symptoms to Watch For: While rare, magnesium deficiency can happen, particularly in people with certain health conditions or those taking specific medications. Symptoms can include muscle cramps, fatigue, irregular heartbeat, and, over time, could potentially impact bone health.
Zinc: The Bone Builder
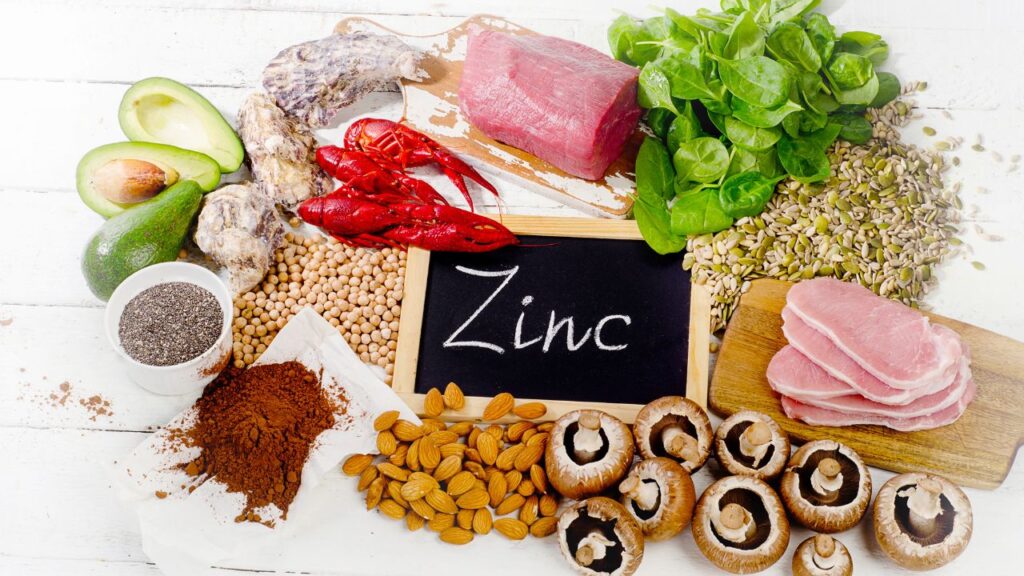
As one of the key trace minerals for bone health, zinc plays a crucial role not only in maintaining bone density and strength but also in overall physical development and immune function. Ensuring adequate zinc intake, either through diet or supplements when necessary, is essential for supporting robust bone health and overall well-being.
Role of Zinc in Bone Health
- Bone Tissue Growth and Repair: Zinc plays a significant role in the growth and repair of bone tissue. It’s a key component in the synthesis of collagen, an essential part of the bone matrix that provides flexibility and strength to bones.
- Bone Density and Strength: It contributes to maintaining bone density and strength. By influencing the bone remodeling process, zinc helps in the formation of new bone and the maintenance of existing bone structure.
- Calcium Absorption and Bone Metabolism: Zinc aids in the absorption of calcium, another critical mineral for bone health. It’s involved in bone metabolism, the process by which bones are continuously renewed and repaired.
Zinc’s Broader Health Benefits
- Immune System Support: Apart from its role in bone health, zinc is well-known for supporting the immune system. It helps in the functioning of immune cells and reduces the risk of infections.
- Wound Healing: Zinc is also essential for wound healing, thanks to its role in collagen synthesis and cell proliferation.
- Overall Growth and Development: For children and adolescents, zinc is vital for growth and development. It’s necessary for cell growth and division, which is especially important during periods of rapid growth.
Sources of Zinc
- Dietary Sources: Zinc can be found in a variety of foods. Meat, particularly red meat and poultry, is a great source. Seafood, especially shellfish like oysters, is rich in zinc. Vegetarian sources include beans, nuts, seeds, and whole grains. Dairy products also provide a good amount of zinc.
- Supplements: Some people may require zinc supplements, especially if their diet lacks sufficient amounts. However, it’s important to be cautious with supplementation, as excessive zinc can interfere with the absorption of other minerals.
Recommended Daily Intake
- Varies Based on Age and Gender: The recommended intake of zinc varies depending on age, gender, and other factors like pregnancy and lactation. For instance, adult men generally need more zinc than adult women.
Zinc Deficiency and Bone Health
- Potential Consequences: Zinc deficiency can lead to impaired bone growth and development, especially in children and adolescents. In adults, it can contribute to bone loss and osteoporosis.
- Identifying Deficiency: Symptoms of zinc deficiency include impaired immune function, hair loss, and delayed wound healing. In severe cases, it can affect bone health.
Boron: The Undercover Bone Agent

Boron is one of the important trace minerals for bone health, playing a pivotal role in mineral metabolism, hormonal balance, and enhancing bone density. Its broader impact on joint and cognitive health further underlines its significance. Incorporating a variety of boron-rich foods into your diet is a simple and effective way to support your bones and overall health.
Boron’s Role in Bone Health
- Mineral Metabolism: Boron is instrumental in the metabolism of key minerals that are crucial for bone health, including calcium, magnesium, and phosphorus. This process is essential for maintaining and building strong bones.
- Bone Density Enhancement: It has been observed that boron can enhance bone density by influencing the way the body handles other minerals and vitamins essential for bone health.
- Hormonal Influence: Boron plays a role in the metabolism of steroid hormones such as estrogen and testosterone, which are important for bone growth and maintenance. It also affects the synthesis of vitamin D, a vital component in bone health.
Wider Health Benefits of Boron
- Joint Health: Beyond bones, boron is beneficial for maintaining healthy joints. It helps reduce inflammation and arthritis symptoms, contributing to overall joint comfort and mobility.
- Cognitive Function: There is evidence to suggest that boron aids in cognitive function, including improving memory and concentration.
Sources of Boron
- Dietary Sources: You can find boron in a variety of foods. Fruits like apples, oranges, and pears, leafy vegetables, nuts, and pulses are good sources. Boron is also present in avocados, potatoes, and even wine.
- Boron Supplements: While getting boron from food is the best option, some people might consider supplements, especially if their diet lacks variety. As always, it’s recommended to consult a healthcare professional before starting any supplement.
Recommended Intake
- No Established RDA: Unlike some other minerals, there is no established Recommended Dietary Allowance (RDA) for boron. However, studies suggest that a daily intake ranging from 1 to 3 mg is beneficial for bone health.
Boron Deficiency and Bone Health
- Signs and Effects: Boron deficiency, while rare, can lead to poorer bone health. This might manifest as reduced bone strength and an increased risk of developing osteoporosis.
- Detection and Management: Recognizing boron deficiency is challenging as the symptoms are not always clear. However, ensuring a diet rich in boron-containing foods can help in maintaining adequate levels.
It’s clear that trace minerals for bone health are not just supplementary; they are fundamental. During perimenopause, a time when women’s bodies undergo significant changes, paying extra attention to bone health becomes crucial. Magnesium, zinc, and boron, among other trace minerals, play a pivotal role in this regard. They ensure that our bones remain strong, resilient, and capable of adapting to the hormonal shifts characteristic of this phase.
Incorporating these minerals into your diet isn’t just about reacting to changes; it’s about proactively supporting your body through its natural evolution. Whether through diet or supplements, ensuring a sufficient intake of these trace minerals can make a significant difference in how you experience perimenopause and your overall bone health.
In essence, the journey through perimenopause is one that can be navigated with grace and vitality, especially when armed with the right knowledge and resources. By understanding and embracing the importance of trace minerals for bone health, you can step into this new chapter of life with confidence, strength, and wellbeing.