10 Practical Ways to Support an Anxious Partner during Perimenopause
When one partner is dealing with anxiety, especially during perimenopause or menopause, the other partner often ends up carrying a lot of emotional weight, which can be pretty draining. Social activities might take a hit because the anxious partner may avoid outings, which can be a bummer if the other partner loves to socialize. Money can also become an issue if anxiety and menopausal symptoms affect job stability, leaving the other partner to pick up the financial slack. Everyday chores like grocery shopping, cooking, and cleaning can pile up on the non-anxious partner, leading to exhaustion and frustration. Over time, these challenges can add up, so it’s crucial to find ways to support your partner and keep things balanced.
Here are some practical ways to help:
1. Educate Yourself
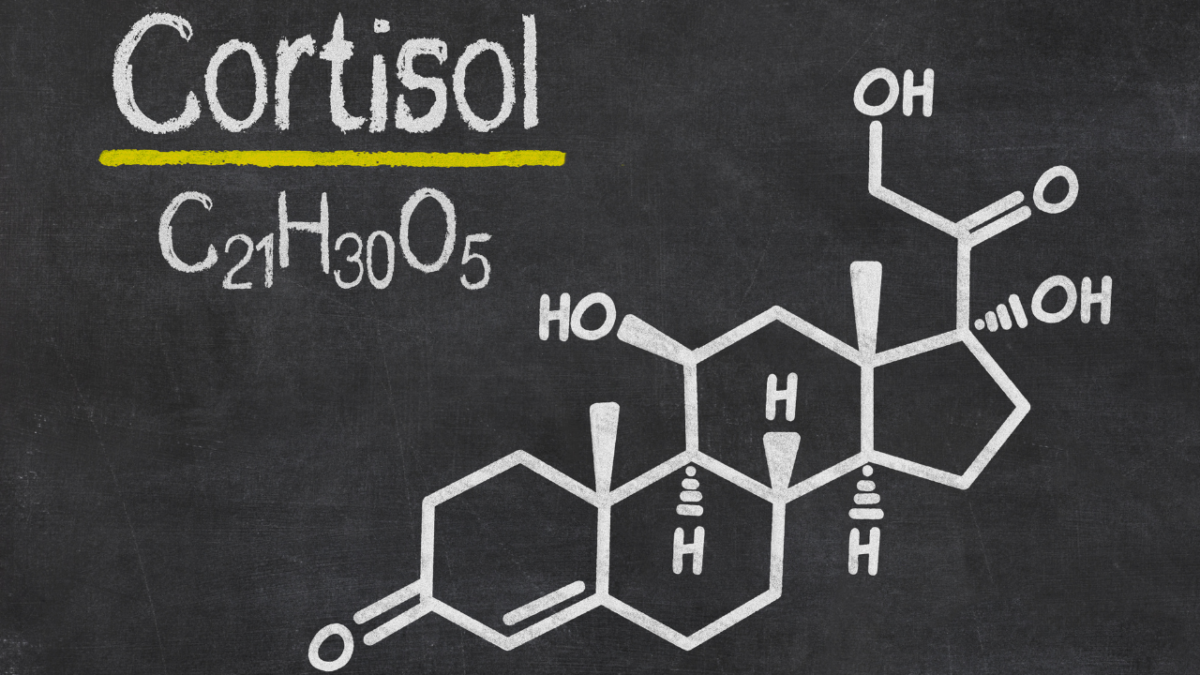
- Learn About Menopause: Understand the symptoms and emotional changes that come with perimenopause and menopause. This knowledge will help you empathize with what your partner is going through.
- Stay Updated: Menopause is a complex process, and symptoms can vary greatly. Regularly seek out new information and resources to stay informed.
2. Open Communication
- Encourage Open Dialogue: Create a safe space for your partner to express her feelings and concerns without judgment. Listen actively and validate her experiences.
- Be Patient: Mood swings and anxiety can make communication challenging. Be patient and avoid reacting negatively.
3. Emotional Support
- Show Empathy: Acknowledge her feelings and let her know you’re there for her. Sometimes, just being present and listening can provide immense comfort.
- Encourage Professional Help: If anxiety becomes overwhelming, gently suggest seeking help from a therapist or counselor who specializes in menopause-related issues.
4. Physical Support
- Exercise Together: Physical activity can help reduce anxiety. Suggesting walks, yoga, or other exercises you can do together can be beneficial.
- Healthy Diet: Encourage a balanced diet rich in vitamins and minerals. Help with meal planning and preparation to ensure she gets the necessary nutrients.
5. Create a Calm Environment
- Reduce Stressors: Identify and minimize stressors in your household. This might include helping with chores, creating a peaceful living space, or managing external pressures.
- Mindfulness Practices: Introduce and practice relaxation techniques together, such as deep breathing exercises, meditation, or mindfulness.
6. Encourage Self-Care
- Promote Relaxation: Encourage activities that your partner finds relaxing, whether it’s a hobby, a bath, reading, or listening to music.
- Sleep Hygiene: Help establish a healthy sleep routine. This includes creating a comfortable sleep environment and encouraging consistent sleep and wake times.
DOWNLOAD THE DAILY SELF-CARE TRACKER HERE
7. Be Flexible and Understanding
- Adapt to Changes: Understand that her needs and preferences might change frequently. Be adaptable and supportive of these changes.
- Offer Reassurance: Regularly reassure your partner of your love and support. Anxiety can sometimes make one feel isolated or unlovable.
8. Practical Help
- Assist with Daily Tasks: Offer to take on more responsibilities around the house to reduce her stress.
- Plan Together: Help her plan and organize her day or week to manage time effectively and reduce feelings of being overwhelmed.
9. Social Support
- Encourage Social Interaction: Encourage her to stay connected with friends and family, which can provide additional emotional support.
- Join Support Groups: Look into local or online support groups for people going through menopause. This can provide a sense of community and shared experiences.
10. Celebrate Small Wins
- Acknowledge Progress: Celebrate small victories in managing anxiety or other symptoms. This positive reinforcement can boost her morale and confidence.
Supporting your partner through perimenopause and menopause involves a combination of understanding, practical help, and emotional support. By taking these steps, you can help alleviate her anxiety and improve her overall well-being.