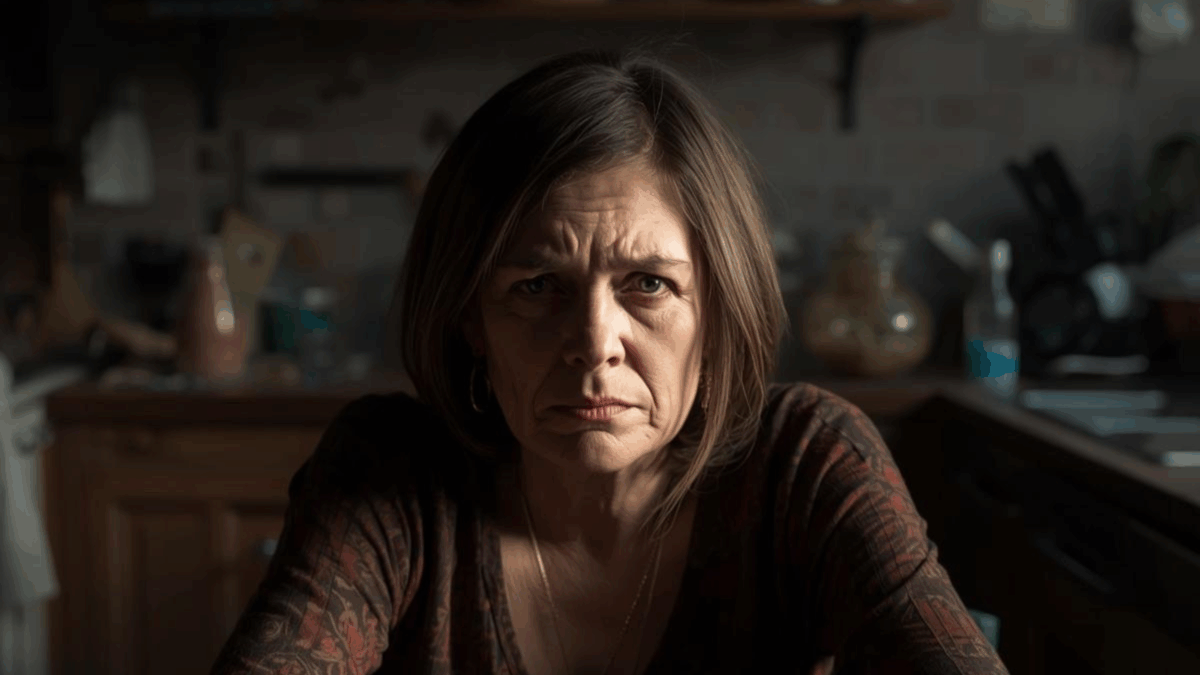
One minute I was discussing sweet potatoes. The next, I was in the bathroom sobbing.
I didn’t used to be this reactive. That’s what I told myself after snapping at my sister over a holiday menu. Or crying in the bathroom after a passive-aggressive comment from my mother. Or storming out of a room I used to feel safe in. It wasn’t just them. It wasn’t just me. Something deeper was happening—something hormonal, emotional, and primal all tangled together.
If this sounds familiar, you’re not alone. And no, you’re not overreacting. You may be navigating a collision between menopause and long-standing family dynamics—two powerful forces that shape our identities and push all our buttons, often at the same time.
This is for every woman who feels like she’s unraveling in front of the people who are supposed to love her. If you’ve ever thought, “Why can’t I handle this like I used to?” — here’s the truth: your body is changing, your emotional wiring is recalibrating, and your tolerance for dysfunction is disappearing. That’s not a breakdown. It’s a reckoning.
Let’s unpack why.
The Hormonal Storm Beneath the Surface
Perimenopause and menopause aren’t just about hot flashes or irregular periods. They’re complex neurological, psychological, and emotional transitions that change how you interpret tone, regulate emotions, and respond to stress.
Estrogen and Emotional Regulation
Estrogen affects the brain’s limbic system—especially the amygdala (your fear and emotion center) and the prefrontal cortex (your reasoning and impulse control hub). When estrogen levels fluctuate, so can:
- Your emotional regulation
- Your sensitivity to stress
- Your capacity for patience
Research shows that estrogen receptors in these areas influence how we experience and manage emotions (Barth, Villringer, & Sacher, 2023).
Progesterone and Your Calming Center
Progesterone, often considered the body’s natural sedative, supports GABA—a neurotransmitter that calms the nervous system. When progesterone drops, you may feel:
- More anxious
- Overwhelmed
- Sleep-deprived (and we all know how sleep deprivation amplifies emotions)
Cortisol and Chronic Stress
When you combine low progesterone, fluctuating estrogen, and high cortisol (the stress hormone), it’s like walking through an emotional minefield. Small comments hit hard. Old wounds feel raw. You may think, “Why am I so sensitive right now?”
Importantly, the menopause transition is recognized as a vulnerable time for mood changes—not just physical ones. Emotional reactivity becomes more common (Harvard Health Publishing, 2023).
When Hormones Meet Family History
Let’s move beyond hormones to the people around you.
When your aunt comments on your weight, or your brother minimizes your exhaustion, it’s rarely about that single moment. It’s about years—sometimes decades—of emotional labor, unspoken pain, and invisible expectations.
Menopause often strips away the emotional filters we once relied on to keep the peace. Things we tolerated for years suddenly feel unbearable. That’s not regression. That’s clarity.
The Invisible Labor of Midlife Women
Midlife women carry the emotional load for everyone:
- Caring for aging parents
- Supporting kids or adult children
- Managing relationships or divorces
- Holding space for others—while quietly burning out
Now your body is asking for something else: rest, recalibration, and radical honesty. That shift alone can rattle family dynamics.
Nina, 52, told me she left Thanksgiving early after her sister made a ‘joke’ about her mood swings. “Ten years ago, I’d have laughed it off. This year? I packed my pie and left.”
When Emotional Flooding Takes Over
Emotional flooding occurs when your nervous system gets overwhelmed. You might:
- Feel hot, dizzy, or flushed
- Want to leave the room
- Struggle to speak
- Cry unexpectedly
- Go completely numb
This isn’t drama. It’s your body saying: “This is too much.”
Research links negative or tense relationships with close family members—especially parents, siblings, or partners—with depressive symptoms and lower psychological well-being in midlife adults (Gilligan, Suitor, Rurka, & Pillemer, 2017).
Why Boundaries Matter More Than Ever
Most of us weren’t raised to set boundaries. We were taught to be nice. To please. To shrink so others could stay comfortable.
But midlife—especially with hormonal upheaval—requires a different approach.
What Boundaries Really Are
Boundaries aren’t walls. They’re filters. They protect your energy, peace, and nervous system.
A boundary might sound like:
- “That comment isn’t helpful.”
- “I’m not available for this conversation right now.”
- “I need some time to myself.”
They are clear, kind, and non-negotiable.
How to Protect Your Emotional Safety Around Family
Here are some powerful ways to support yourself during triggering moments:
1. Anticipate Your Triggers
- Know your “hot buttons”
- Decide ahead how you’ll respond
- Let someone safe help support you
2. Use Grounding Tools in Real Time
- Press your feet into the floor
- Put a cold object on your neck or wrist
- Breathe in for 4, hold for 4, exhale for 6
3. Give Yourself Permission to Leave
- Step away. Take a walk. Decline the invite. Presence isn’t a performance.
4. Don’t Explain Boundaries to People Who Benefit From You Not Having Them
- If someone keeps crossing the line, you don’t owe them endless explanations. State it once. Hold it firmly.
When the Drama Comes from Inside the House
Sometimes, it’s not your aunt or cousin. It’s your partner. Your grown child. Your parent living in the guest room.
Even the most loving relationships can feel strained when menopause enters the mix. Hormonal shifts, identity changes, and physical symptoms ripple into intimacy, communication, and patience.
Emotion regulation isn’t one-size-fits-all. We manage emotions differently depending on the relationship—whether with a parent, partner, or sibling. That’s why close family interactions can hit harder (Günther & Baucom, 2021).
You’re not wrong for needing more softness, space, or solitude.
Support Is Out There
- Consider couples or family therapy
- Try guided apps like Paired or Lasting
- Use “I feel __ when __ because __” to clarify emotions without blaming
What Healing Actually Looks Like
Healing in menopause isn’t about everyone suddenly treating you better. It’s about:
- Trusting your instincts
- Honoring your emotional signals
- Grieving what’s no longer working—without guilt
- Making peace with being misunderstood by people unwilling to grow
You’re not hard. You’re clear.
This Chapter Is Yours to Rewrite
Menopause is more than biology—it’s a reset. A chance to:
- Decide how you’re treated
- Stop over-explaining your needs to people who won’t listen
- Choose relationships that honor your growth—not guilt you into old roles
So let your triggers teach you—not trap you.
Let your anger guide you—not consume you.
And let your changing body lead you—toward peace, not performance.
Your Next Step
If family dynamics feel unbearable lately, start here:
- Name your top three triggers
- Set one boundary
- Practice nervous system safety
- Seek therapy or community support
You’re not broken. You’re transforming. And this version of you? She’s not angry—she’s awake.
Disclaimer: This blog is for informational purposes only and is not intended to replace medical advice, diagnosis, or treatment. Please consult your healthcare provider before making decisions about hormone therapy, mental health treatments, or lifestyle changes. Everyone’s experience with menopause is unique, and personalized care is essential.
References
Barth, C., Villringer, A., & Sacher, J. (2023). Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Brain Sciences, 15(9), 1003. https://doi.org/10.3390/brainsci15091003
Gilligan, M., Suitor, J. J., Rurka, M., & Pillemer, K. (2017). Family networks and psychological well-being in midlife. Research in Human Development, 14(1), 18–33. https://doi.org/10.1080/15427609.2017.1285865
Günther, A., & Baucom, B. R. (2021). Emotion regulation in close relationships: The role of individual and relational factors. Frontiers in Psychology, 12, 697901. https://doi.org/10.3389/fpsyg.2021.697901
Harvard Health Publishing. (2023). Menopause and mental health. Harvard Health.https://magazine.hms.harvard.edu/articles/mental-health-aspects-menopause