Migraine vs. Tension Headache: What’s the Difference?
Menopause-related headaches are often due to hormonal fluctuations in the body. Estrogen levels, in particular, play a significant role. As these levels fluctuate and eventually decline, many women experience an increase in headache frequency and intensity, especially those with a history of migraines. Two primary types of headaches are commonly associated with menopause:
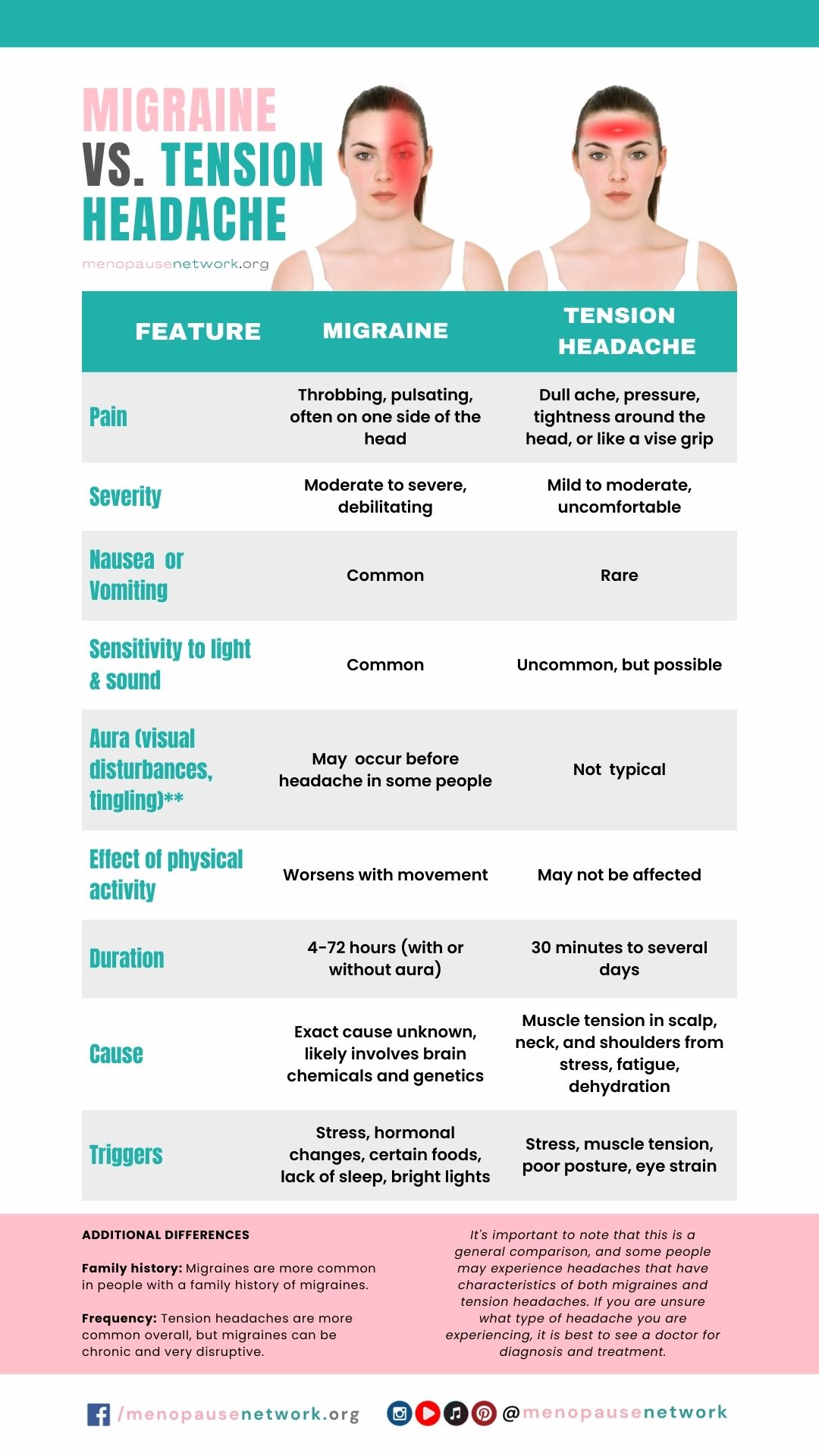
- Migraines: These can become more frequent or severe during perimenopause and menopause. Migraines are typically characterized by throbbing pain on one side of the head, sensitivity to light and sound, and sometimes nausea and vomiting.
- Tension Headaches: Often described as a feeling of pressure around the head, tension headaches are also common and may be related to stress, anxiety, or depression, which can be exacerbated by menopause.
Understanding the type of headache you’re experiencing is crucial for finding effective treatment and relief.
Lifestyle Modifications
Diet and Hydration
Diet plays a critical role in managing menopause-related headaches. Incorporating a diet rich in fruits, vegetables, whole grains, and lean proteins can help stabilize hormones and reduce inflammation, potentially alleviating headache symptoms. It’s essential to stay hydrated by drinking plenty of water throughout the day, as dehydration can be a significant headache trigger. Additionally, identifying and avoiding specific dietary triggers—such as caffeine, alcohol, aged cheeses, and processed foods—can also help prevent headache episodes.
Exercise
Regular physical activity is beneficial not only for overall health but also for reducing the frequency and severity of headaches. Exercise helps release endorphins, the body’s natural painkillers, and reduces stress, a common trigger for headaches. Aim for at least 30 minutes of moderate exercise most days of the week. Activities like brisk walking, cycling, swimming, or yoga can be particularly effective and enjoyable.
Sleep
Quality sleep is essential for headache management. Hormonal changes during menopause can disrupt sleep patterns, leading to insomnia and, consequently, increased headache frequency. Establishing a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime can improve sleep quality and reduce headaches.
Stress Management
Menopause can be a stressful time, and stress is a well-known trigger for headaches. Developing stress-reduction techniques is crucial for managing menopause-related headaches. Practices such as yoga, meditation, deep breathing exercises, and progressive muscle relaxation can significantly reduce stress levels and the likelihood of headache occurrence.
Medical Interventions
Hormone Replacement Therapy (HRT)
HRT can be an effective treatment for reducing menopausal symptoms, including headaches, by stabilizing hormone levels. However, it’s not suitable for everyone and carries potential risks, such as an increased risk of blood clots and certain cancers. Discussing the benefits and risks of HRT with a healthcare provider is crucial to make an informed decision.
Prescription Medications
For those experiencing severe or frequent menopause-related headaches, especially migraines, prescription medications may offer relief. Medications such as triptans are effective for treating migraines, while preventative medications like beta-blockers, calcium channel blockers, or antidepressants can reduce the frequency of headaches. A healthcare provider can recommend the most appropriate medication based on individual symptoms and medical history.
Over-the-counter Remedies
For occasional, mild headaches, over-the-counter (OTC) pain relievers like ibuprofen, aspirin, or acetaminophen can be effective. However, it’s important to use these medications judiciously to avoid overuse, which can lead to rebound headaches.
Alternative Therapies and Supplements
Acupuncture and Chiropractic Care
Acupuncture and chiropractic adjustments can offer relief for some individuals experiencing menopause-related headaches. These alternative therapies may help reduce headache frequency and severity by improving blood flow, reducing muscle tension, and promoting relaxation.
Here’s a video that shows the 7 Pressure Points To Relieve Your Headache
Herbal Supplements and Vitamins
Certain supplements and vitamins may help reduce the frequency and severity of migraines and other headaches. Magnesium, riboflavin (vitamin B2), and Coenzyme Q10 have shown promise in reducing migraine frequency. Herbal supplements such as feverfew and butterbur may also offer relief, but it’s important to consult with a healthcare provider before starting any new supplement, especially for individuals taking other medications.
When to See a Doctor
If menopause-related headaches become more frequent, severe, or change in pattern, consulting a healthcare provider is essential. Symptoms that require immediate medical attention include headaches accompanied by fever, stiff neck, seizures, confusion, double vision, weakness, or difficulty speaking. Keeping a headache diary that tracks the frequency, duration, severity, and potential triggers of headaches can be invaluable for diagnosis and treatment.
Personal Care and Support Networks
During menopause, focusing on self-care and mental health is crucial. Engaging in activities that bring joy and relaxation can improve overall well-being and potentially reduce headache frequency. Building a support network of friends, family, and support groups can provide emotional support and practical advice for managing menopause and its symptoms, including headaches.
Takeaway
Navigating menopause-related headaches requires a holistic approach, combining lifestyle changes, medical interventions, and alternative therapies tailored to individual needs and preferences. By understanding the triggers and types of headaches, individuals can empower themselves to find relief and improve their quality of life during menopause. It’s important to remember that support is available, and consulting healthcare professionals can provide guidance and treatment options to effectively manage menopause-related headaches.




