Why Am I So Angry Lately? The Hidden Hormonal and Emotional Roots of Rage in Perimenopause
Why Am I So Angry Lately? The Hidden Hormonal and Emotional Roots of Rage in Perimenopause
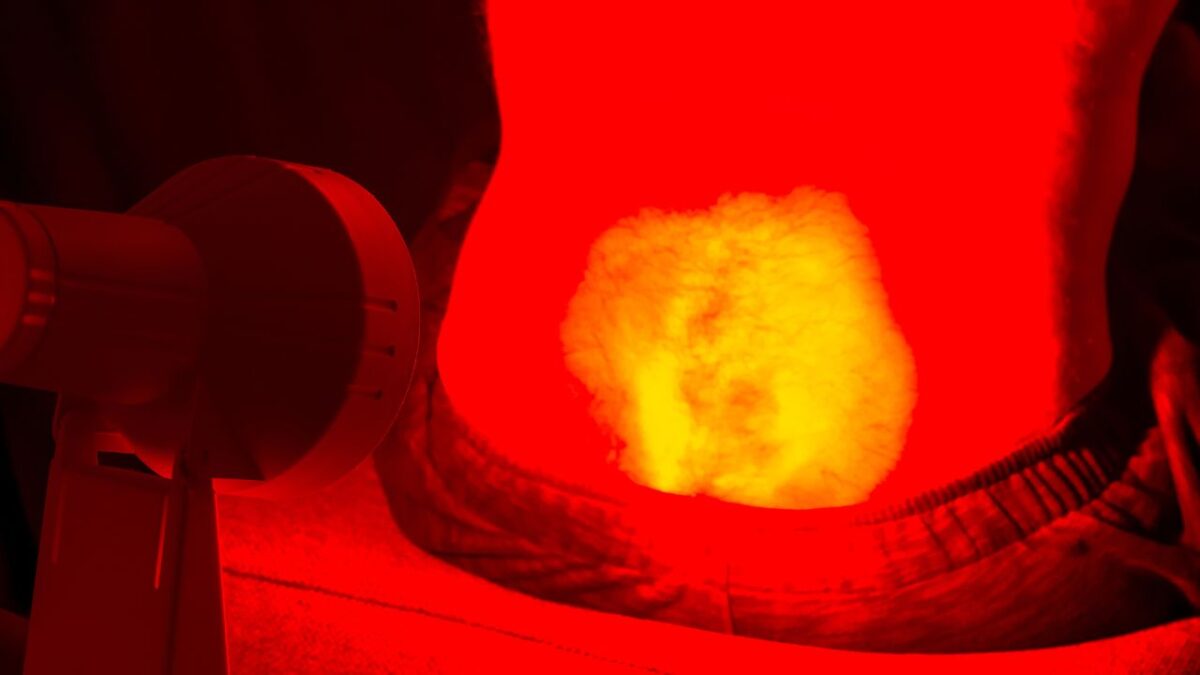
I used to think I was just stressed out. Work deadlines, a cluttered kitchen, a partner who couldn’t seem to find the laundry basket—minor irritations that suddenly felt volcanic. But this wasn’t just stress. This was something else. Something deeper, louder, and harder to control.
If you’ve been asking yourself, “Why am I so angry lately? Why does everything set me off?” — you’re not alone. And no, you’re not just being dramatic. There’s a very real, biological reason that your emotional thermostat has gone haywire.
This isn’t about being ungrateful or out of control. This is about perimenopause.
The Emotional Earthquake No One Warned Us About
Perimenopausal rage doesn’t always look like screaming. Sometimes it’s an internal boil—a simmering frustration that bubbles beneath every interaction. Other times it’s explosive, surprising even you. And what’s worse? No one seems to talk about it.
Lisa, 46, told me, “I love my kids. But suddenly their chewing makes me want to scream. I don’t recognize myself anymore.”
These moments aren’t character flaws. In fact, they’re hormonal flags waving for attention.
The Science of Why You’re So Angry
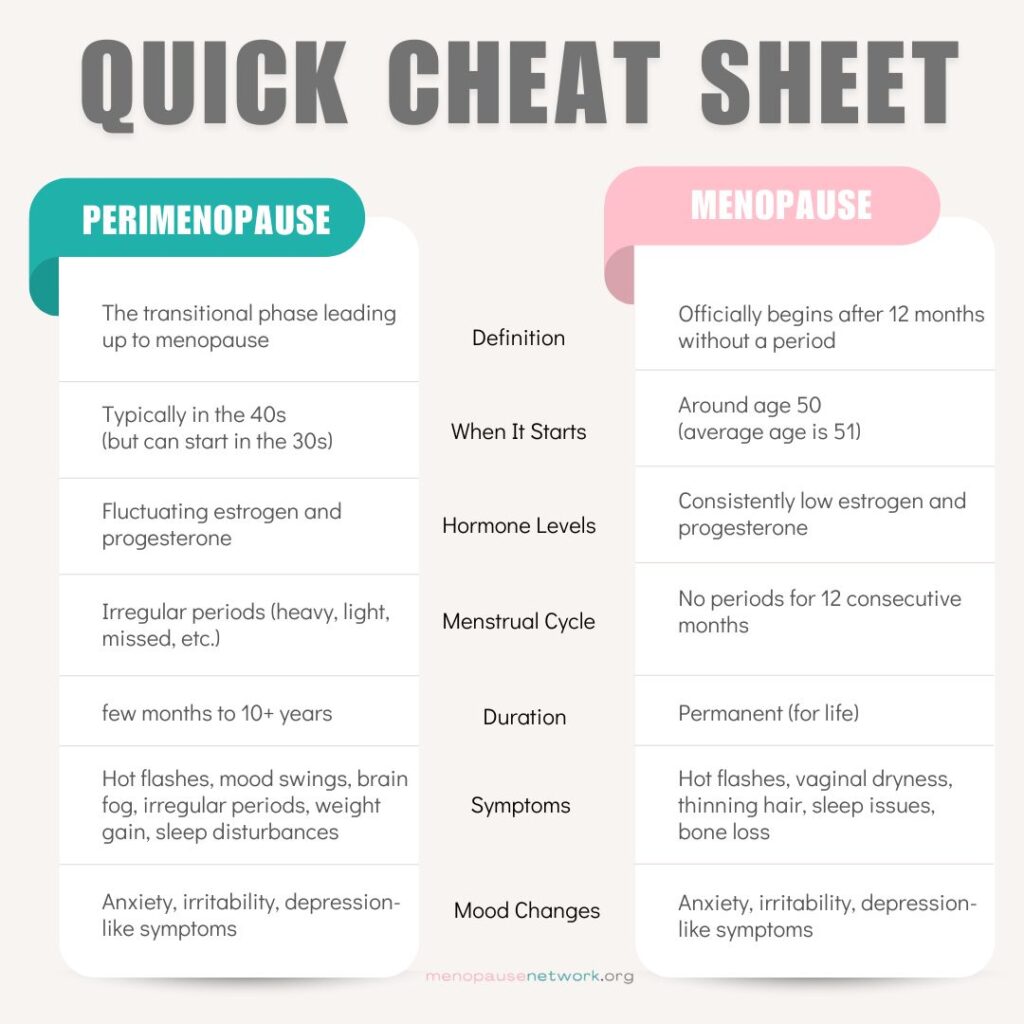
Estrogen’s Rollercoaster
Estrogen doesn’t just regulate your reproductive system—it also plays a role in mood. It supports serotonin, the brain’s feel-good chemical, and helps modulate cortisol, your stress hormone.
During perimenopause, estrogen levels spike and crash unpredictably. These fluctuations can affect:
- Mood stability
- Stress response
- Emotional regulation
Sudden estrogen dips may contribute to sudden mood shifts in some women (Harvard Health Publishing, 2023; The Menopause Charity, 2023).
Progesterone’s Disappearing Act
Progesterone, often considered a calming hormone, tends to decline faster than estrogen during perimenopause. Some emerging research suggests this may contribute to anxiety or emotional sensitivity in certain individuals, though the connection isn’t fully understood (ScienceDirect, 2023).
Cortisol: The Amplifier
Cortisol, your body’s primary stress hormone, becomes harder to regulate during menopause transitions. While fluctuating estrogen can affect mood, high cortisol levels may amplify emotional overreactions.
Hormonal instability during perimenopause may affect the neurochemical pathways that govern emotional control (ScienceDirect, 2023).
It’s Not Just Hormones—It’s Life
Perimenopause often collides with peak life stress:
- Aging parents
- Teen children
- Career pivots or burnout
- Sleep disruption
- Relationship strain
These pressures intensify emotional reactivity. While hormones may light the fuse, life often loads the cannon (Healthline, 2023).
The Hidden Cost of Suppressing Anger
Many women are conditioned to be “nice,” to not make waves. But unexpressed anger doesn’t disappear—it turns inward. It can manifest as:
- Anxiety
- Depression
- Physical tension
- Chronic fatigue
You’re not failing if you’re angry—instead, you’re responding to a changing internal and external landscape.
What Rage Is Really Trying to Tell You
Rage is a signal. It’s not just about what’s happening now—it’s the cumulative weight of:
- Feeling invisible
- Carrying everyone else’s load
- Neglecting your own needs
- Not being heard
Menopause doesn’t invent these feelings. Rather, it makes them louder.
Science-Backed Ways to Soothe the Fire
1. Track Your Mood and Cycle
Even if periods are irregular, tracking your mood daily can help you spot patterns. Apps like Balance, Me v PMDD, or even a journal can help you correlate emotional spikes with hormonal shifts (Healthline, 2023).
2. Nourish Your Nervous System
- Prioritize sleep (even if it means naps)
- Eat to stabilize blood sugar
- Try adaptogens like ashwagandha or rhodiola (with medical guidance)
- Reduce alcohol and caffeine
3. Move—But Gently
Exercise helps metabolize stress hormones, but overdoing it can raise cortisol. Instead, opt for:
- Walking
- Yoga
- Dance
- Strength training with rest days
4. Reframe the Rage
What if anger wasn’t a flaw—but a message?
- What boundary is being crossed?
- What need is unmet?
- Where are you overextending?
Therapists trained in Internal Family Systems (IFS) or somatic therapy can help you explore rage as a protective response—not a character defect.
5. Get Medical Support
- Hormone therapy may help stabilize mood symptoms as part of a broader symptom management plan, especially when other menopausal symptoms are present (BMJ Clinical Review, 2023).
- SSRIs or SNRIs may be recommended for mood-related symptoms, particularly if there’s a pre-existing mood disorder (Mass General Brigham, 2023).
- Some women find micronutrients like magnesium or omega-3s supportive, though clinical research on their effectiveness during perimenopause is still developing (Harvard Health Publishing, 2023).
Talk to a provider who understands menopause—not one who dismisses it.
Your Relationships Might Need a Reset Too
Anger doesn’t just affect you. It changes the tone of partnerships, parenting, and professional relationships. When your fuse is shorter:
- Communicate your experience to loved ones
- Use “I” statements (“I’ve been feeling overwhelmed and short-fused lately”)
- Set boundaries without guilt
Re-educating your circle is part of reclaiming your wellbeing.
Anger Isn’t the Enemy—Disconnection Is
This stage of life is often misunderstood, but it’s also an invitation: to reconnect with yourself, to re-establish your needs, and to express what’s been silenced for too long.
You are not too much. You are not broken. You are not alone. You are transforming.
This isn’t the end of who you were—it’s the beginning of who you’re becoming.
Your Next Step
If you’ve felt hijacked by rage, don’t dismiss it. Instead, explore it. Listen to it. And get support.
- Track your mood
- Talk to your doctor
- Get therapy if it’s accessible
- Join a support group
You deserve care. You deserve peace. You deserve to be heard.
Disclaimer: This blog is intended for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you’re experiencing intense mood changes, emotional distress, or considering hormone therapy or mental health support, please consult a qualified healthcare provider. Every woman’s experience with perimenopause is different, and personalized care is essential for finding what works best for you.
References
- Harvard Health Publishing. (2023). Menopause and mental health. https://www.health.harvard.edu/womens-health/menopause-and-mental-health
- ScienceDirect. (2023). Mood disorders and hormonal fluctuations in midlife women. https://www.sciencedirect.com/science/article/pii/S0378512224001828
- Healthline. (2023). Perimenopause rage: Why it happens and how to cope. https://www.healthline.com/health/menopause/perimenopause-rage
- ACOG. (2022). Mood changes during perimenopause. https://www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know
- Mass General Brigham. (2023). Menopause and mental health. https://www.massgeneralbrigham.org/en/about/newsroom/articles/menopause-and-mental-health
- The Menopause Charity. (2023). Menopause and mental health. https://themenopausecharity.org/information-and-support/symptoms/menopause-and-mental-health
- BMJ. (2023). Menopause and the role of hormone therapy: clinical review. https://www.bmj.com/content/bmj/382/bmj-2022-072612.full.pdf