Menopause Got You Feeling Electric? Here’s How to Cope!
Hot flashes, night sweats, and mood swings are the usual menopause symptoms, but some women experience something more unusual and startling—sensations that feel like electric shocks. If you’ve ever wondered why you feel tiny zaps, you’re not alone. Let’s explore this lesser-known symptom of menopause and how you can manage it.
What Causes Electric Shock Sensations During Menopause?
The sensation of electric shocks can be a bewildering and unsettling experience. These zaps are typically short, sharp, and often occur just before a hot flash. While they may seem alarming, there’s a scientific explanation behind them.
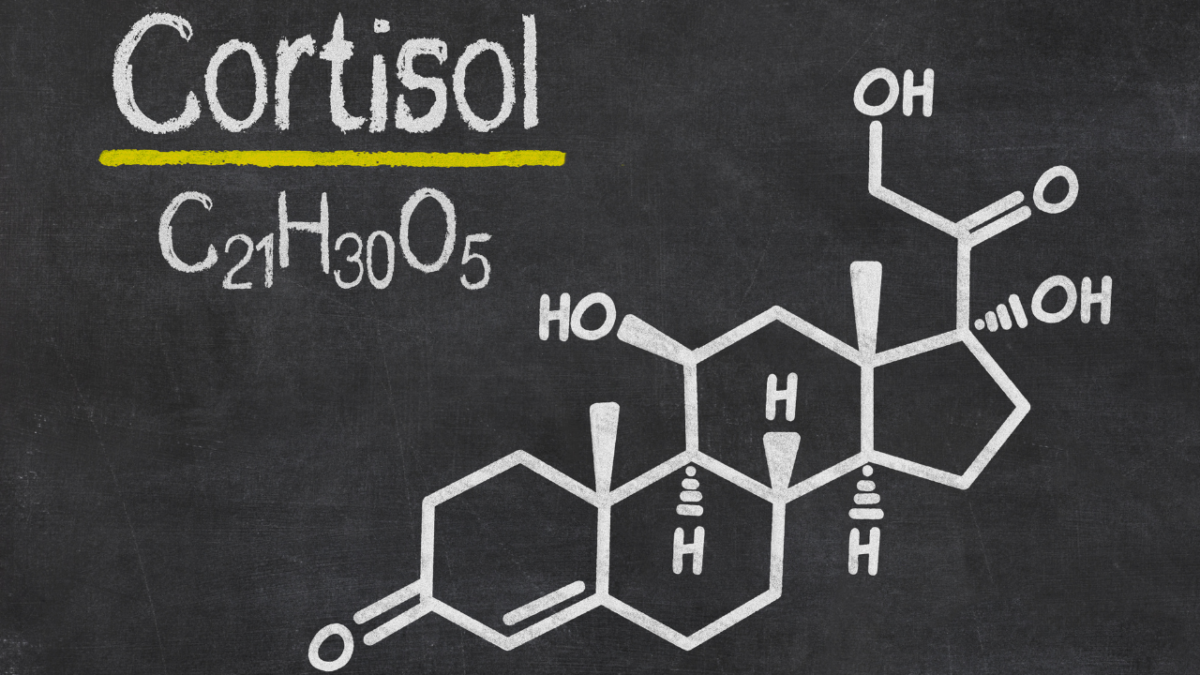
Hormonal Changes: During menopause, your body undergoes significant hormonal fluctuations, particularly in estrogen levels. These hormonal shifts can affect the nervous system, leading to unusual sensations, including the feeling of electric shocks.
Neurological Factors: Menopause doesn’t just affect your reproductive system; it can also impact your central and peripheral nervous systems. Research has looked into these electric shock sensations, linking them to neurological and sensory issues. A 2022 study found that those zaps can increase the risk of several neurological diseases and symptoms affecting both the central and peripheral nervous systems. These can include epilepsy, convulsions, headaches, and disturbances of skin sensation, among other symptoms. Hormonal changes might increase the sensitivity of your sensory nerves, making you more susceptible to these electric sensations.
Electrodermal Activity: Studies have shown that hot flashes are associated with changes in electrodermal activity—essentially, how your skin reacts to electrical conductance. These changes can cause sensations of heat and, occasionally, electric shocks due to sudden surges in skin conductance.
Long-Term Neurological Effects
While the immediate sensation of an electric shock is brief, some women may worry about long-term effects. Research has found that electric shocks, particularly if frequent, can be associated with various neurological conditions. Here are some key findings:
- Increased Risk of Neurological Disorders: Studies indicate that women experiencing frequent electric shocks during menopause might have a higher risk of developing conditions like epilepsy, migraines, and neuropathy.
- Cognitive Impacts: Long-term exposure to hormonal fluctuations can affect cognitive functions. Research shows a potential link between menopause-related electric shocks and issues like memory lapses, brain fog, and even depression.
- Peripheral Nerve Sensitivity: As your body adjusts to new hormone levels, you might find that your nerves become more sensitive. This can lead to increased incidents of electric shock sensations and other neuropathic symptoms.
Managing Neurological Symptoms
The good news is that there are several strategies you can adopt to manage and reduce these unsettling sensations. Here are some practical tips to help you cope:
- Stay Cool: Since electric shocks often precede hot flashes, keeping cool can help. Wear light, breathable clothing, use fans, and keep your environment at a comfortable temperature.
- Healthy Diet: A balanced diet rich in vitamins and minerals can support your nervous system. Incorporate foods high in B vitamins, magnesium, and omega-3 fatty acids to help maintain nerve health.
- Stay Hydrated: Dehydration can exacerbate neurological symptoms. Ensure you’re drinking plenty of water throughout the day to keep your body and nervous system hydrated.
- Regular Exercise: Physical activity can help regulate your hormones and improve your overall well-being. Aim for regular exercise, such as walking, yoga, or swimming, to keep your body active and reduce symptoms.
- Stress Management: Stress can worsen neurological symptoms. Practice relaxation techniques such as deep breathing, meditation, or mindfulness to help manage stress levels.
- Medical Treatments: If your symptoms are severe, consider speaking to your healthcare provider about medical treatments. Hormone Replacement Therapy (HRT) or other medications might be an option to help balance your hormones and reduce symptoms.
- Electro-Acupuncture: Some studies suggest that electro-acupuncture can be beneficial in managing menopausal symptoms, including electric shocks. This treatment involves using acupuncture needles with a small electrical current and may help regulate nerve activity.
When to Seek Professional Help
While many women can manage these symptoms with lifestyle changes and self-care, it’s important to know when to seek professional help. If you experience frequent or severe electric shocks, or if they are accompanied by other symptoms like significant pain, numbness, or cognitive issues, consult your healthcare provider. They can conduct thorough evaluations to rule out other conditions and provide personalized treatment options.
Takeaway
Menopause can be a wild ride, with surprises around every corner. Those electric shock sensations, though unsettling, are just another part of the journey for some women. By understanding the causes and implementing effective management strategies, you can navigate these symptoms with confidence. Remember, you’re not alone, and with the right approach, you can reduce these sensations and enjoy a better quality of life during menopause.
Additional Resources
For more information and support, consider joining menopause support groups, consulting with a menopause specialist, or exploring educational resources online. Knowledge is power, and staying informed can help you take charge of your menopausal journey.