A Day in the Life of a Perimenopausal Woman: Balancing the Highs and Lows
Perimenopause hits every woman a bit differently. It’s a whirlwind of hormonal shifts, physical changes, and emotional ups and downs. For many, it can feel like a wild rollercoaster ride – unpredictable and sometimes overwhelming. But amidst the hot flashes, mood swings, and sleepless nights, there are also moments of resilience, humor, and self-discovery.
In this article, we’ll take you through a day in the life of a perimenopausal woman, showcasing real-life scenarios and daily struggles. From early morning battles with night sweats to midday brain fog, we’ll face each challenge with a mix of empathy and lightheartedness. We’ll follow her routine from the first groggy moments of dawn to the quiet self-care rituals at night.
But this article isn’t just about sharing experiences. It also aims to provide valuable tips for managing perimenopausal symptoms, helping those in this stage of life find ways to cope. By focusing on small, actionable steps, we aim to empower women to take charge of their health and well-being during this transformative time. From smart dietary choices and lifestyle tweaks to simple tricks for staying cool and collected, these tips are here to make each day a little easier. Plus, we hope to bring some positive vibes and humor to lighten an already challenging day.
Join us as we explore the daily life of a perimenopausal woman, celebrating her strength and resilience. Whether you’re on this journey yourself or supporting someone who is, this story is a reminder that you’re not alone. Together, we can navigate the ups and downs of perimenopause with grace, humor, and a shared sense of sisterhood.
6:00 AM – The Early Bird’s Dilemma
The alarm clock buzzes. You wake up, not because you’re well-rested, but because you’re too hot to sleep. Hello, night sweats! After peeling off the sheets, you head to the bathroom for your morning ritual, hoping a cold splash of water will revive you. Your reflection shows thinning hair and a new wrinkle that wasn’t there yesterday. You smile at yourself, knowing beauty isn’t just skin deep.
I know waking up drenched in night sweats is no fun and can feel incredibly frustrating. Your body is going through some significant changes right now, and it’s perfectly normal to feel overwhelmed. First, remember to keep a fan by your bedside and wear moisture-wicking pajamas to stay cool during the night. And when it comes to your morning reflection, remember that every line and change is a part of your unique story.
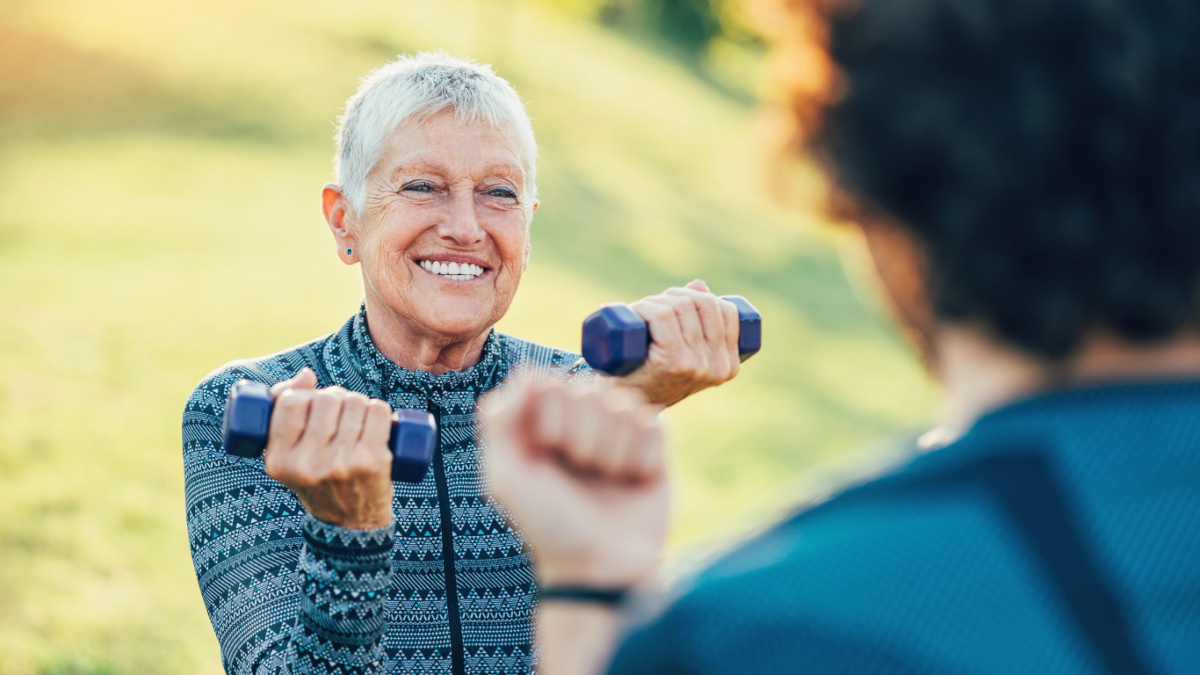
Thinning hair can be tough to see, but there are treatments and styles that can help you feel more like yourself. Embrace the changes with grace and patience; your beauty truly shines from within. Focus on your overall well-being – a balanced diet, staying hydrated, and gentle exercise can all make a huge difference.
7:00 AM – Breakfast with a Side of Fog
Breakfast is an adventure. Did you put the coffee in the toaster? Oh no!!! Yo forgot! No worries, these little mishaps are all part of the experience. You’ll do great by sticking to healthy choices like yogurt and flaxseed – those omega-3s are fantastic for your overall health.
It’s smart to stay on top of your vitamin D supplement, especially since it can help with mood and bone health. And when it comes to the ‘meno-fog,’ you’re not alone. Mental clarity can come and go, but you’re managing it well by jotting down reminders. Sticky notes are a lifesaver, and they’ll help you keep track of your daily tasks and important to-dos.
9:00 AM – The Morning Hustle
Work starts, and so do the hot flashes. Your office mate jokes that it’s like working in the tropics. It’s great that you can laugh it off with your colleagues – a sense of humor can be a powerful ally during this phase. But let’s focus on some strategies to help you feel more comfortable.
Consider dressing in layers, so you can easily adjust your clothing to stay cool. Keeping a handheld fan at your desk is a smart idea, and yes, a small personal air conditioner or cooling towel could be a worthwhile investment if the hot flashes are frequent.
Remember to stay hydrated throughout the day and take short breaks to walk around and cool down. It’s impressive that you power through your work despite the discomfort – it shows your resilience and determination. If hot flashes continue to be a significant issue, we can discuss some treatment options that might help manage the symptoms more effectively.
12:00 PM – Lunch and Learn
Lunchtime is a perfect opportunity to recharge, and you’re making excellent choices with that salad. Leafy greens, nuts, and a light vinaigrette are packed with nutrients that can help support your overall well-being. Sharing a laugh with colleagues and discussing helpful tips, like herbal teas for calming nerves, is a wonderful way to build a supportive network.
It’s great to see you connecting with others and finding comfort in these moments. A strong support system can make a significant difference during perimenopause. Embrace these connections and allow yourself to lean on them when needed.
Remember to savor these lighter moments and continue exploring foods and teas that make you feel good.
3:00 PM – Afternoon Slump
The post-lunch slump hits hard. You feel an overwhelming urge to nap, but instead, you take a brisk walk around the block. The fresh air and movement boost your energy levels. Returning to your desk with a handful of almonds and some green tea is a smart choice, as both can help sustain your energy and keep you focused.
It’s wonderful that your resilience and strength shine through in moments like these. Remember to be kind to yourself and acknowledge the effort you’re putting into managing these symptoms.
If the slumps continue to be a challenge, you can explore additional strategies together with your doc, like adjusting your diet or incorporating more short breaks into your day.
6:00 PM – Homeward Bound
The workday ends, but the responsibilities don’t. Dinner needs to be made, and the kids need help with homework. You opt for a simple, healthy meal – grilled chicken, quinoa, and steamed veggies. As you sit down with your family, you relish the moments of connection and the support they offer, even if they don’t fully understand what you’re going through.
Remember, it’s okay to ask for help and delegate tasks when needed. Sharing responsibilities can lighten your load and provide you with more time for self-care. You’re doing an amazing job juggling all these roles, and your strength and resilience are truly inspiring.
9:00 PM – Wind Down
Never underestimate the power of small, peaceful moments. Taking time for yourself is incredibly important, especially during perimenopause. A warm bath with lavender oil is a wonderful way to soothe your senses and relax. It’s great to hear that you’re setting a calming bedtime routine – reading a book and creating a peaceful environment can significantly improve your sleep quality.
It’s okay if you don’t get perfect rest every night. What’s important is that you cherish and prioritize these moments of tranquility. Consistency in your bedtime routine can help signal to your body that it’s time to wind down, which can gradually improve your sleep over time.
Throughout the Day – Moments of Self-Compassion
Throughout the day, remember to be kind to yourself. Practice self-compassion and find humor in the daily struggles. Celebrate the small victories, no matter how minor they may seem, and find humor in the little mishaps. These moments of joy and laughter are powerful tools for maintaining a positive outlook.
You’re navigating this phase with an admirable blend of grace and resilience. Each step you take, no matter how challenging, is a testament to your strength and determination. Remember that showing kindness to yourself is not just important; it’s essential. It allows you to recharge and face each new day with renewed energy.
Perimenopause is like an unpredictable wave, but with the right approach, you can navigate it with grace. From night sweats to brain fog, each day brings challenges and victories, showcasing your resilience.
Celebrate the little wins and be kind to yourself. Practical tips like healthy meals, staying active, and calming routines make a big difference. Lean on your support network and seek professional advice when needed.
This unique adventure is filled with unexpected turns. By keeping a sense of humor and a proactive attitude, you can turn perimenopause into a time of growth and self-discovery.
Embrace the ride, find joy in the small moments, and discover your incredible strength.